360 Suite of Services

PORA redefines overpayment oversight with intelligent automation. Leveraging proprietary algorithms, machine learning, and secure API architecture, it equips healthcare organizations with the tools to identify anomalies, validate claims, and manage audits with accuracy, speed, and confidence.
Full-Scope Overpayment Management
Built-In Intelligent Algorithms
Proprietary algorithms and machine learning models automatically analyze claims data, pinpoint anomalies, and prioritize high-value cases. This enables faster detection, stronger recoveries, and smarter audit decisions.
Secure, Seamless Deployment
PORA - Advanced Audit Automation
Our flagship solution streamlines provider communications and enables bulk validation processing with built-in algorithms and pricing logic.
Automated Letter Generation & Tracking
PORA streamlines provider communications with built-in letter generation and automated tracking. From notifications to follow-ups, every step is logged and auditable, ensuring compliance and reducing manual effort.
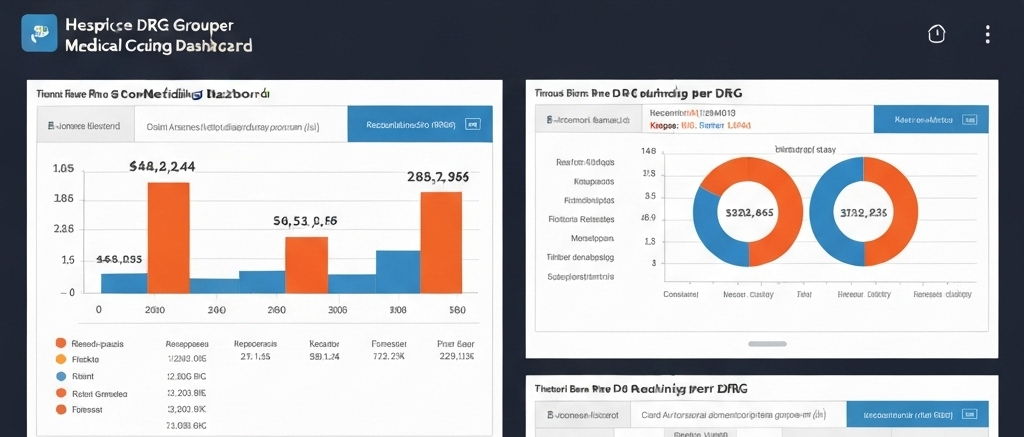
Bulk Validation & Processing
PORA enables auditors to validate and process large volumes of claims at once, applying built-in algorithms and pricing logic in bulk. This capability reduces manual review time, increases efficiency, and ensures consistent, accurate results across every case.
Task Assignment & Oversight
Assign cases to auditors, track progress in real time, and ensure accountability across your audit team. PORA’s task management tools make collaboration seamless and transparent.

What PORA Delivers
- Billing anomaly detection
- Case tracking and audit workflows
- Automated letter generation
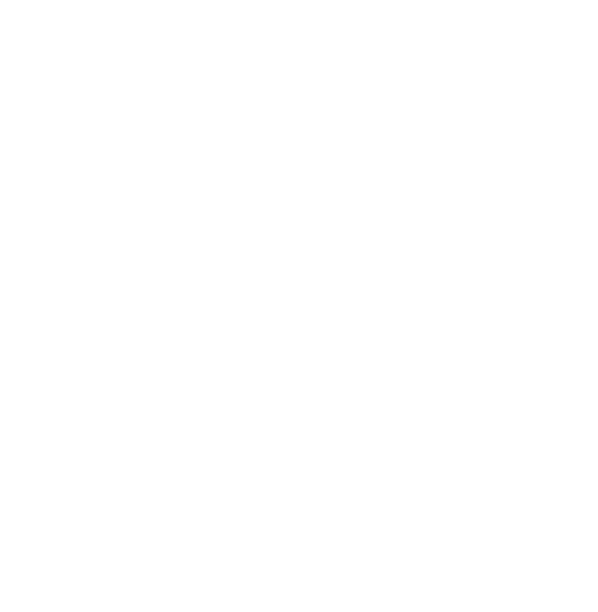
- Configurable dashboards and reports
- Secure data management
- Easy integration with existing systems
Complete Payment Integrity Suite
The 360 Health Systems Payment Integrity Suite is a portfolio of specialized applications designed to help healthcare organizations strengthen audit accuracy, optimize workflows, and protect revenue. Each application is built to address a critical dimension of payment integrity from advanced audit automation with PORA, to intelligent pricing and grouping with the DRG Grouper & Pricer, and ongoing Algorithm Research & Development that drives continuous innovation. Together, these tools deliver a comprehensive, technology-first approach to detecting overpayments, accelerating recoveries, and supporting long-term operational resilience.

Algorithm Research and development
DRG Grouper & Pricer
Complex Audit

Vendor Portal
Automated Letter Generation & Tracking
PORA streamlines provider communications with built-in letter generation and automated tracking. From notifications to follow-ups, every step is logged and auditable, ensuring compliance and reducing manual effort.
Bulk Validation & Processing
PORA enables auditors to validate and process large volumes of claims at once, applying built-in algorithms and pricing logic in bulk. This capability reduces manual review time, increases efficiency, and ensures consistent, accurate results across every case.
Task Assignment & Oversight
Assign cases to auditors, track progress in real time, and ensure accountability across your audit team. PORA’s task management tools make collaboration seamless and transparent.
Task Assignment & Oversight
Assign cases to auditors, track progress in real time, and ensure accountability across your audit team. PORA’s task management tools make collaboration seamless and transparent.
Key Benefits
Discover how PORA can transform your payment integrity operations
and deliver exceptional value.
Increased Recovery
Reduced Waste
Time Savings
Improved Accuracy
Actionable Insights
We continuously evolve our technology to
stay ahead of industry challenges.
Enhanced Collaboration
Ready to Transform Your Payment Integrity?
Schedule a demo to see how 360 Health Systems can help you recover lost revenue and reduce financial waste.
Ready to See PORA in Action?
Schedule a Demo to see how our comprehensive payment integrity
solution can help you recover lost revenue and reduce financial waste.